As sciatica progresses, it can enter its last stages, presenting unique challenges and symptoms. Understanding these final phases is crucial for effective management and treatment.
Here’s what you need to know:
1. Persistent Pain: In the last stages of sciatica, pain often becomes more persistent and may even intensify. This constant discomfort can significantly impact daily life and mobility.
2. Muscle Weakness: As the condition progresses, muscle weakness in the affected leg may become more pronounced. This weakness can affect balance, stability, and overall function.
3. Nerve Damage: Prolonged compression of the sciatica nerve can lead to nerve damage, causing tingling sensations, numbness, or loss of sensation in the affected leg.
4. Exacerbation of Symptoms: In the last stages of sciatica, symptoms may exaggerate, with sharp, shooting pains becoming more frequent and intense.
5. Limited Mobility: Severe sciatica can severely limit mobility, making it difficult to perform everyday activities such as walking, standing, or sitting for extended periods.
6. Bowel or Bladder Control Issues: In rare cases, advanced sciatica may lead to bowel or bladder control issues, known as cauda equina syndrome. This condition requires immediate medical attention.
7. Treatment Challenges: Treating sciatica in its last stages can be challenging, as the underlying cause may be more complex and require surgical intervention or specialized treatments.
Understanding the last stages of sciatica empowers individuals to seek appropriate treatment and management strategies to alleviate symptoms and improve quality of life.
Managing Sciatica Pain: Symptoms and Solutions
Sciatica pain can be debilitating, affecting mobility and quality of life. Understanding the symptoms and exploring effective solutions are essential for managing this condition.
Here’s what you need to know:
Recognizing Symptoms:
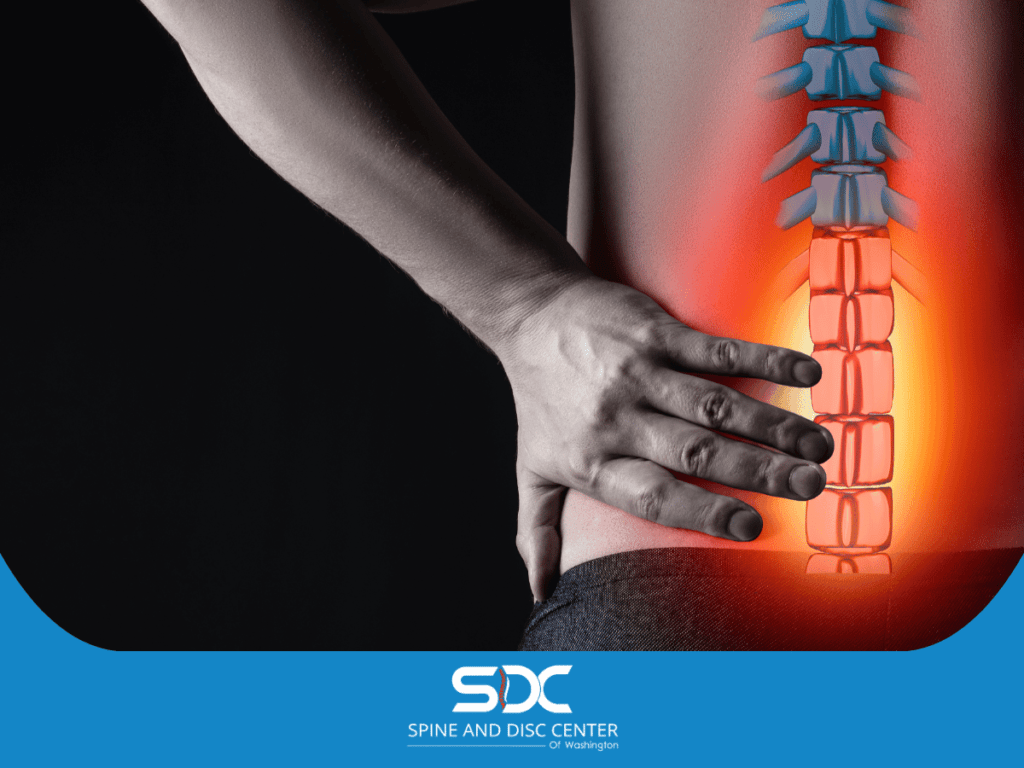
Sciatica pain typically manifests as a shooting or burning sensation that radiates along the path of the sciatica nerve from the lower back down the back of one leg.
Other common symptoms include numbness, tingling, or weakness in the affected leg.
Seeking Relief:
If you’re experiencing sciatica pain, there are several strategies you can try to alleviate discomfort. These include:
- Hot and Cold Therapy: Applying heat or ice packs to the affected area can help reduce inflammation and relieve pain.
- Over-the-Counter Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or acetaminophen can help alleviate pain and reduce inflammation.
- Physical Therapy: Working with a physical therapist to perform targeted exercises and stretches can help improve flexibility, strengthen muscles, and alleviate pressure on the sciatica nerve.
- Chiropractic Care: Spinal adjustments and manipulations performed by chiropractors can help realign the spine, alleviate nerve compression, and reduce sciatica pain.
- Massage Therapy: Massage techniques such as deep tissue massage or trigger point therapy can help relax tight muscles, improve circulation, and reduce pain associated with sciatica.
Lifestyle Modifications:
Making certain lifestyle changes can also help manage sciatica pain. These include:
- Maintaining Good Posture: Practicing proper posture can help alleviate pressure on the spine and reduce sciatica symptoms.
- Avoiding Prolonged Sitting: Sitting for extended periods can aggravate sciatica pain. Take regular breaks to stretch and move around throughout the day.
- Using Proper Body Mechanics: When lifting heavy objects or bending down, use your legs instead of your back to reduce strain on the spine.
- Incorporating Low-Impact Exercise: Engaging in activities such as swimming, walking, or yoga can help strengthen muscles, improve flexibility, and reduce sciatica pain.
When to Seek Medical Attention:
While many cases of sciatica pain can be managed with self-care measures, it’s essential to seek medical attention if you experience:
- Severe or persistent pain: If sciatica pain is severe, persistent, or worsening over time, it may indicate a more serious underlying condition that requires medical evaluation.
- Loss of bowel or bladder control: This could be a sign of cauda equina syndrome, a rare but serious condition that requires immediate medical attention.
Collaborating with Healthcare Professionals:
Working closely with healthcare professionals, such as chiropractors, primary care physicians, orthopedic specialists, or physical therapists, can help develop a comprehensive treatment plan tailored to your individual needs.
Exploring Sciatic Nerve Compression and Its Effects
Sciatic nerve compression, often associated with conditions like herniated discs or spinal stenosis, can lead to a range of debilitating symptoms.
Understanding the causes and effects of sciatic nerve compression is crucial for effective management.
Here’s what you need to know:
Understanding Sciatic Nerve Compression:
The sciatic nerve is the longest nerve in the body, running from the lower back down the back of each leg. When pressure is placed on it, the sciatic nerve compresses, often due to conditions such as herniated discs, spinal stenosis, or muscle tightness.
Common Causes of Compression:
Several factors can contribute to nerve compression, including:
- Herniated Discs: When the soft inner core of a spinal disc protrudes through the tough outer layer, it can press on the nearby sciatic nerve roots, causing compression and pain.
- Spinal Stenosis: This condition occurs when the spinal canal narrows, putting pressure on the spinal cord and nerve roots, including the nerve.
- Muscle Tightness: Tight muscles in the buttocks or lower back can compress the sciatic nerve, leading to sciatica symptoms.
Effects of Sciatic Nerve Compression:

Sciatic nerve compression can result in a variety of symptoms, including:
- Pain: The most common symptom of sciatic nerve compression is pain that radiates from the lower back down the leg. This pain may be sharp, shooting, or burning in nature.
- Numbness and Tingling: Compression of the nerve can cause numbness, tingling, or a pins-and-needles sensation in the buttocks, leg, or foot.
- Muscle Weakness: In severe cases of sciatic nerve compression, muscle weakness or difficulty moving the affected leg may occur.
- Difficulty Standing or Walking: Sciatica pain and associated symptoms can make standing, walking, or performing daily activities challenging.
Sciatica Treatment Options:
Treatment for sciatic nerve compression aims to alleviate pain, reduce inflammation, and relieve pressure on the affected nerve.
Sciatica treatment options may include:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or corticosteroids may be prescribed to reduce pain and inflammation.
- Physical Therapy Exercises: Targeted exercises and stretches can help improve flexibility, strengthen muscles, and alleviate pressure on the sciatic nerve.
- Chiropractic Care: Spinal adjustments and manipulations performed by chiropractors can help realign the spine, alleviate nerve compression, and reduce sciatica pain.
- Injections: Epidural steroid injections or nerve blocks may be recommended to deliver anti-inflammatory medication directly to the affected area and provide pain relief.
Surgical Intervention:
In cases where conservative treatments fail to provide relief, surgical intervention may be considered to address the underlying cause of sciatic nerve compression, such as removing a herniated disc or widening the spinal canal.
Preventive Measures:
To help prevent sciatic nerve compression, it’s essential to maintain good posture, practice proper lifting techniques, and engage in regular exercise to strengthen the muscles supporting the spine.
By understanding the causes and effects of sciatic nerve compression and exploring appropriate treatment options, individuals can effectively manage symptoms and improve their quality of life.
Consult a healthcare professional for personalized evaluation and treatment if you’re experiencing persistent or severe nerve compression symptoms.
Treating Chronic Sciatica: From Diagnosis to Recovery
Chronic sciatica, characterized by persistent pain along the sciatic nerve, can significantly impact daily life. Understanding the diagnosis and treatment options is essential for effectively managing this condition and achieving recovery. Here’s a comprehensive guide:
Diagnosis of Chronic Sciatica:
Diagnosing chronic sciatica typically involves a thorough medical history review, physical examination, and diagnostic tests, including:
- Medical History: Your healthcare provider will inquire about your symptoms, medical history, and any factors contributing to sciatica, such as recent injuries or underlying health conditions.
- Physical Examination: A physical examination may include tests to assess muscle strength, reflexes, and sensation in the affected leg, as well as maneuvers that reproduce sciatica symptoms.
- Imaging Studies: Imaging tests such as X-rays, MRI scans, or CT scans may be ordered to visualize the spine and identify underlying causes of sciatic nerve compression, such as herniated discs or spinal stenosis.
Conservative Treatment Options:
In many cases, conservative treatments are effective in managing chronic pain and promoting sciatica recovery. These may include:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or neuropathic pain medications may be prescribed to alleviate severe pain and inflammation.
- Physical Therapy: Targeted exercises, stretches, and manual therapy techniques can help improve flexibility, strengthen muscles, and alleviate pressure on the sciatic nerve.
- Chiropractic Care: Spinal adjustments and manipulations performed by chiropractors can help realign the spine, reduce nerve compression, and alleviate sciatica symptoms.
- Heat and Cold Therapy: Applying heat or cold packs to the affected area may help reduce inflammation, alleviate pain, and promote the relaxation of tight muscles.
Interventional Procedures:
If conservative treatments fail to provide relief, interventional procedures may be recommended to target pain and inflammation directly. These may include:
- Epidural Steroid Injections: Corticosteroid injections into the epidural space around the spinal cord can help reduce inflammation and provide temporary pain relief.
- Nerve Blocks: Injection of a local anesthetic or medication directly into the affected nerve root can help block pain signals and provide relief.
Surgical Intervention:
In severe cases of chronic sciatica that do not respond to conservative treatments or interventional procedures, surgical intervention may be considered. Surgical options may include:
- Discectomy: Surgical removal of a herniated disc that is compressing the nerve.
- Laminectomy: Surgical removal of part of the vertebra to relieve pressure on the spinal cord and nerve roots.
- Spinal Fusion: Fusion of two or more vertebrae to stabilize the spine and reduce movement that may be causing nerve compression.
Recovery and Rehabilitation:
Following treatment, rehabilitation efforts focus on restoring function, improving mobility, and preventing future episodes of sciatica. Physical therapy, targeted exercises, and lifestyle modifications may be recommended to support recovery and prevent recurrence.
Long-Term Management:
Chronic sciatica requires ongoing management to minimize symptoms and maintain quality of life. This may include regular exercise, proper posture, weight management, and stress reduction techniques.
Understanding the diagnosis and treatment options for chronic sciatica can help individuals take proactive steps to manage their condition, alleviate symptoms, and promote recovery.
If you’re experiencing symptoms persistent of chronic sciatica, consult with a healthcare professional for personalized evaluation and treatment.
The Role of Physical Therapy in Sciatica Rehabilitation

Physical therapy is crucial in rehabilitating sciatica, helping individuals regain function, alleviate pain, and improve overall quality of life.
Here’s how physical therapy can benefit those recovering from sciatica:
1. Pain Management: Physical therapists utilize various techniques to help manage sciatica pain, including manual therapy, therapeutic exercises, and modalities such as heat or cold therapy. These interventions aim to reduce inflammation, alleviate muscle tension, and decrease severe pain intensity.
2. Improving Range of Motion: Sciatica often restricts movement and flexibility in the spine and affected leg. Physical therapy includes targeted exercises and stretches designed to improve the range of motion in the lumbar spine and hip joints, promoting better mobility and function.
3. Strengthening Weak Muscles: Sciatica can lead to muscle weakness due to reduced activity and nerve compression.
Physical therapists develop personalized exercise programs to strengthen muscles in the lower back, hips, and legs, helping support the spine and prevent future injury.
4. Correcting Posture and Body Mechanics: Poor posture and body mechanics can exacerbate sciatica symptoms.
Physical therapists teach proper body mechanics and ergonomic principles to reduce strain on the spine and promote optimal alignment, reducing the risk of re-injury.
5. Education and Self-Management: Physical therapists educate individuals about their condition, teaching them how to recognize triggers, manage symptoms, and prevent flare-ups. They provide guidance on ergonomic modifications, lifestyle changes, and home exercises to support long-term recovery.
6. Functional Nerve Rehabilitation: Physical therapy focuses on restoring functional abilities necessary for daily activities and returning to work or recreational activities. Therapists tailor rehabilitation programs to address specific functional deficits and goals, helping individuals regain independence and confidence.
7. Preventing Recurrence: Physical therapy aims to prevent the recurrence of sciatica episodes through targeted exercise, education, and lifestyle modifications.
By addressing underlying biomechanical issues and promoting proper movement patterns, physical therapists empower individuals to maintain spinal health and reduce the risk of future injury.
At-home Care Strategies During Recovery
While professional treatment is essential for managing sciatica, at-home care strategies can complement recovery efforts and promote healing. Here are some effective strategies to incorporate into your daily routine:
- Heat and Ice Therapy: Alternating between heat and ice packs can help reduce inflammation and alleviate pain associated with sciatica. Apply a heat pack to the affected area for 15-20 minutes followed by an ice pack for another 15-20 minutes, repeating this cycle several times a day.
- Gentle Stretching Exercises: Performing gentle stretching exercises can help improve flexibility and reduce muscle tension in the lower back and legs. Focus on stretches that target the hamstrings, hip flexors, and piriformis muscles to relieve pressure on the sciatic nerve.
- Proper Posture: Maintaining good posture is crucial for relieving pressure on the spine and reducing sciatic pain. Avoid slouching when sitting or standing and use ergonomic chairs and lumbar support cushions to support your lower back.
- Rest and Relaxation: Adequate rest is essential for healing your body from sciatica. Ensure you get enough sleep each night and incorporate relaxation techniques such as deep breathing, meditation, or yoga into your daily routine to reduce stress and tension in the muscles.
- Over-the-counter Pain Relief: Over-the-counter pain relievers such as ibuprofen or acetaminophen can help alleviate mild to moderate sciatic pain. However, always consult with your healthcare provider before taking any medication, especially if you have existing medical conditions or are taking other medications.
- Healthy Lifestyle Choices: Adopting a healthy lifestyle can support your body’s natural healing processes and reduce the risk of recurrent sciatic pain. Eat a balanced diet rich in fruits, vegetables, lean proteins, and whole grains, stay hydrated, and avoid smoking and excessive alcohol consumption.
- Stay Active: While rest is essential during the acute phase of sciatica, staying active can help prevent stiffness and promote circulation. Engage in low-impact activities such as walking, swimming, or cycling, and gradually increase your activity level as tolerated.
By incorporating these at-home care strategies into your daily routine, you can support your recovery from sciatica and minimize the risk of future flare-ups. However, if your symptoms persist or worsen despite home treatment, consult your healthcare provider for further evaluation and guidance.
Contact a Chiropractor for Sciatic Pain Management
When seeking effective sciatic pain management, chiropractors are primary healthcare professionals well-equipped to provide comprehensive care.
Through spinal adjustments, they address misalignments that may be compressing the sciatic nerve, offering drug-free pain relief and promoting natural healing processes.
Chiropractors tailor treatment plans to each patient, focusing on alleviating pain, improving mobility, and restoring overall spinal health.
If you’re experiencing sciatic pain, scheduling a consultation with a chiropractor can be a proactive step toward finding lasting relief and enhancing your quality of life.
Common Questions Asked to Spine Specialists
What Causes Sciatica?
Sciatica is typically caused by compression or irritation of the sciatic nerve, often due to a herniated disc, spinal stenosis, or degenerative disc disease.
What Are the Symptoms of Sciatica?
Common symptoms of sciatica include pain, numbness, tingling, or weakness that radiates from the lower back down the leg, often on one side of the body.
How Is Sciatica Diagnosed?
Sciatica is diagnosed through a combination of physical examination, medical history review, and diagnostic tests such as X-rays, MRI, or CT scans to identify the underlying cause of symptoms.
What Are the Treatment Options for Sciatica?
Treatment for sciatica may include conservative measures such as rest, physical therapy, medication, or epidural steroid injections. In some cases, surgical intervention may be necessary to alleviate nerve compression.
How Long Does Sciatica Pain Last?
The duration of sciatica pain can vary depending on the underlying cause and severity of symptoms. In many cases, symptoms resolve within a few weeks with conservative treatment, while chronic sciatica may require ongoing management.
Can Sciatica Be Prevented?
While it’s not always possible to prevent sciatica, maintaining a healthy lifestyle, practicing good posture, and avoiding activities that strain the spine can help reduce the risk of developing sciatic nerve pain.
When Should I See a Spine Specialist?
It’s advisable to consult with a spine specialist if you experience persistent or severe sciatica symptoms that interfere with daily activities or if symptoms worsen despite conservative treatment measures.
Conclusion
In conclusion, this blog post aims to provide valuable information regarding sciatica. However, it’s essential to recognize that every individual’s situation is unique and accurate diagnosis and tailored treatment are crucial for effective management.
Therefore, if you’re experiencing sciatica symptoms or have concerns about your spinal health, we encourage you to schedule an appointment with our specialist.
Our team is dedicated to providing personalized care and comprehensive solutions to help you find relief and improve your quality of life.